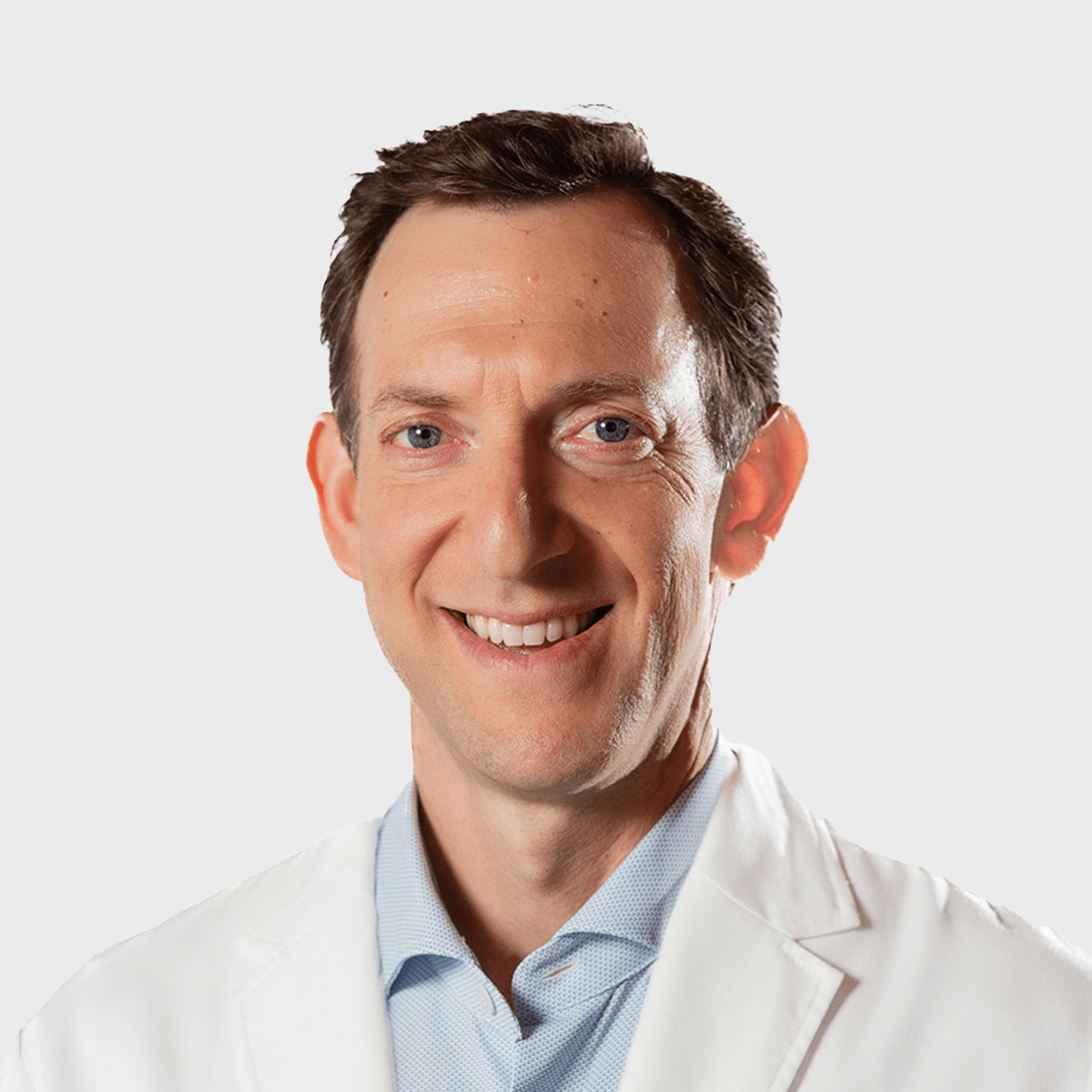
Featured Doctor
David J. Hergan, MD
Get to know Dr. David Hergan, joint replacement and sports medicine surgeon at Middlesex Orthopedic & Spine Associates.
View Profile
Learn more about orthobiologics and regenerative medicine in a Q&A with Dr. David Hergan, orthopedic surgeon at MOSA:
What is regenerative medicine?
Regenerative medicine, or orthobiologics, uses a patient’s own biology to treat certain conditions in a more natural way. Orthobiologics can help avoid or delay surgical intervention as well as be an adjunct to help improve surgical outcomes. Two of the most common orthobiologics are platelet-rich plasma (PRP) and bone marrow aspirate concentrate (BMAC) therapies.
What’s the difference between PRP and BMAC?
PRP is derived from a patient’s own blood, while BMAC is harvested from a patient’s bone marrow. Through these mechanisms we can harness the body’s own regenerative powers to promote healing and increase function.
When compared to PRP, BMAC has higher concentrations of growth factors and even some live stem cells. Patients are often a better candidate for BMAC if they have more advanced arthritic joints such as osteoarthritis of the knee. If you have mild arthritis or need a boost to heal with tendinopathies, then PRP might be more appropriate. While BMAC is more invasive as it comes from your bone marrow versus your blood, it’s still an in-office procedure under local anesthesia.
Has there been any clinical research on regenerative medicine?
Regenerative medicine has grown as a field over recent years. More clinical research is being done than ever before demonstrating its effectiveness as a powerful treatment option for more and more orthopedic conditions. Data has shown the efficacy of both PRP and BMAC in treating osteoarthrosis in many joints, particularly in the knee. It’s been shown to improve symptoms and increase healing for other orthopedic conditions such as partial thickness rotator cuff tears, tendinopathies and ligament injuries. Furthermore, it’s also effectively used as an adjunct to surgery. Studies have shown that getting a PRP injection while in the operating room for a rotator cuff repair or ligament reconstruction can help improve tendon-to-bone healing.
What do you like best about regenerative medicine as a treatment option?
As an orthopedic surgeon, I often see patients who are experiencing joint pain yet may not be good candidates for surgery – or do not want surgery. There are certain patients that either do not experience sufficient results with the standard treatment options or are not good surgical candidates. We previously told these patients to either just live with their pain or wait until it gets worse. This is not acceptable to me. I want to be able to offer my patients more innovative options. Orthobiologics allows me to effectively achieve this goal. Now, I can offer my patients an alternative to surgery that has no additives. By definition, orthobiologics are the most natural treatment as it comes from the patient’s own body. I’ve seen benefits to patients of all ages from high school athletes all the way up to older adults with arthritic knees who want to avoid joint replacements.
Why should I come to MOSA for regenerative medicine treatments?
At MOSA, we are strategically positioned in the middle of Connecticut between New York City and Boston. I see many patients who are seeking regenerative medicine treatments and can’t find them locally and resort to going out of state or even traveling internationally. I’ve thoroughly researched the best ways to perform PRP injections, as not all centrifuge machines are created equal. We’ve found the most effective equipment on the market that can harness the greatest number of platelets once the blood is drawn. The more platelets that can be delivered to the area of disease, the more nutrients that can be delivered, thus the more growth factors and greater potential benefits. Just as importantly, we have a group of highly-trained orthopedic surgeons with years of specialty surgical training experience to perform the injections.
While regenerative medicine is still considered ‘experimental’ by the FDA and typically not covered by insurance, there are many clinical trials showing it can change lives for the better.
What’s next in regenerative medicine?
I believe regenerative medicine is the next frontier of orthopedics. In the past few decades, orthopedic advancements improved the implants we use. I think that in this decade, orthobiologics will be the answer to a lot of our questions about the most effective disease-modifying treatments and potentially even disease-reversing agents! Beyond PRP and BMAC, stem cell therapies such as adipose fat and exosomes are starting to be used clinically.